A 63 year old male patient resident of marripeda bangla
- Get link
- X
- Other Apps
OA 63 year old male patient residence of Marripeda bangla came with
Cheif Complaints:-
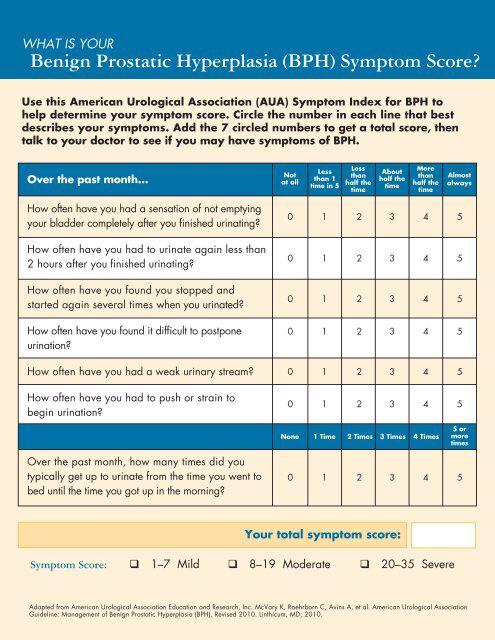
Complaints of increased frequency of passage of urine since one month.
Complaints of fever since 1 month
Back pain since 15 days
Vomiting Since one day
History of presenting illness
Patient was apparently aAsymptomaticsymptomatic one month back then he developed burning micturition which was insidious in onset, no aggravating and relieving factors
Complaints of increased frequency of urine approximately 20 times a day and increased passage of urine during night Times approximately 5 times since 1 month.
fever was insidious in onset, gradually progressive ,intermittent , associated with chills and rigors, low grade, relieved on medication
Back pain sudden in onset dull aching which started after fall from the accident.
Complaints of vomiting since one day, non projectile, non bilious 4 episodes, food as content
Complaints of shortness of breath since 5 days
Patient feels Dehydrated since 5 days
No history of cold and cough
No history of chest pain, palpitation ,syncope
Past history
History of RTA 1 year back, where he got admitted in the hospital used medication for diabetes, continued for 3 months, stopped by the patient as he felt alright after using the medication for 3 months,from then he has knee pains.
History of Roaf traffic accident 15 days back started to develop body pains since then
Uses NSAIDs daily to relieve the pain
No history of similar complaints in the past
No history of hypertension,epilepsy , asthma, TB
Personal history
Patient works in a garage as a daily worker
He maintain normal diet
He sleep is adequate
Patient has constipation since 15 days, passes stools after 4 days, passes only after using medication
Bladder moments increased frequency of passage of urine since 1 month
Addictions consumes alcohol occasionally
Family history
No significant family history
General examination
Patient was conscious, cooperative, coherent
No pallor, icterus,cyanosis,lympadenopathy,edema of foot
Scars over the right hand on dorsal region,scar on shin of right and left lower tibia
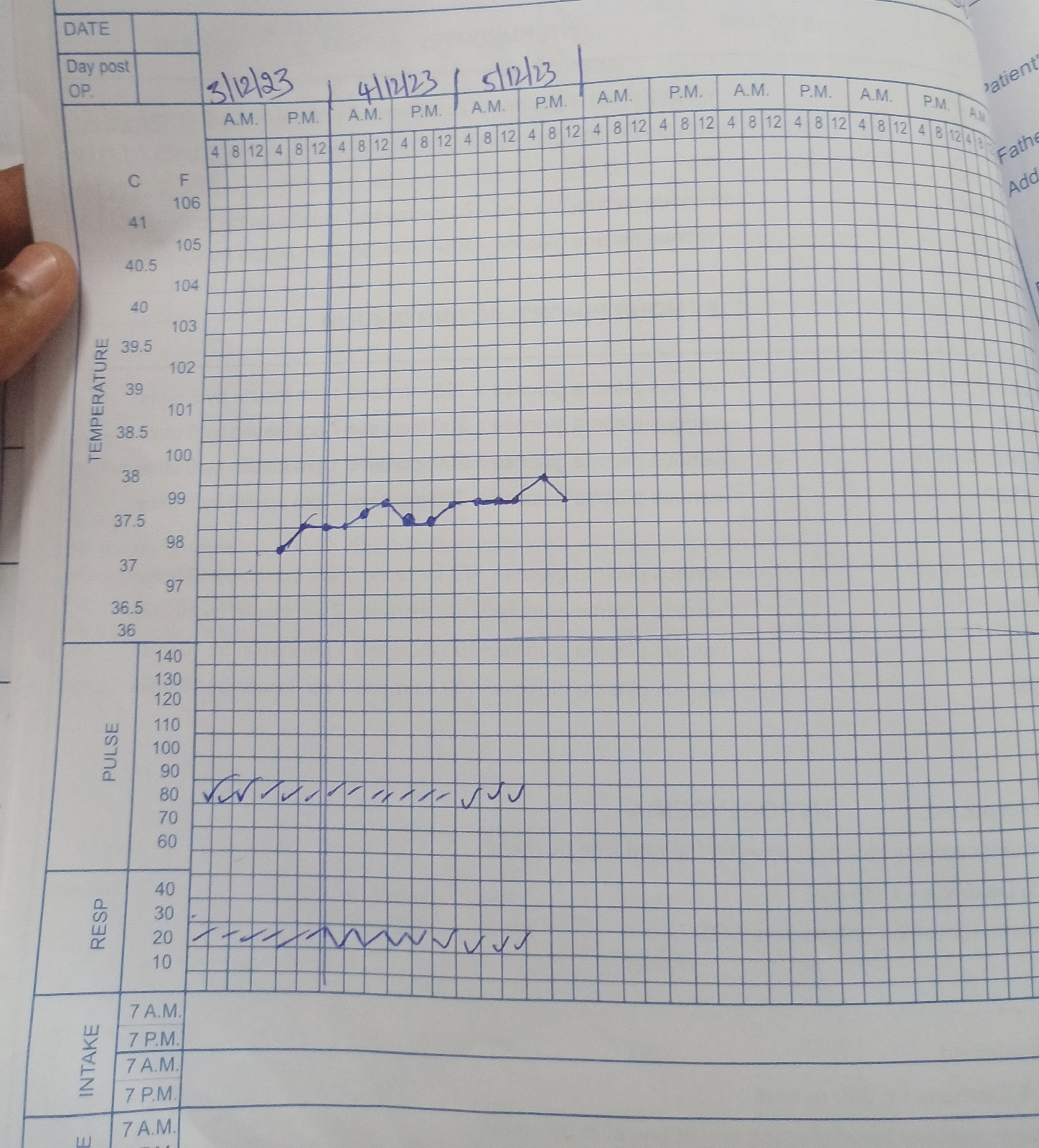
Vitals on presentation
Temp:- 99.5F
Pr:- 108 bpm
Rr:- 30 cpm
Bp:-120/70 mmHg
Spo2:- 97% on RA
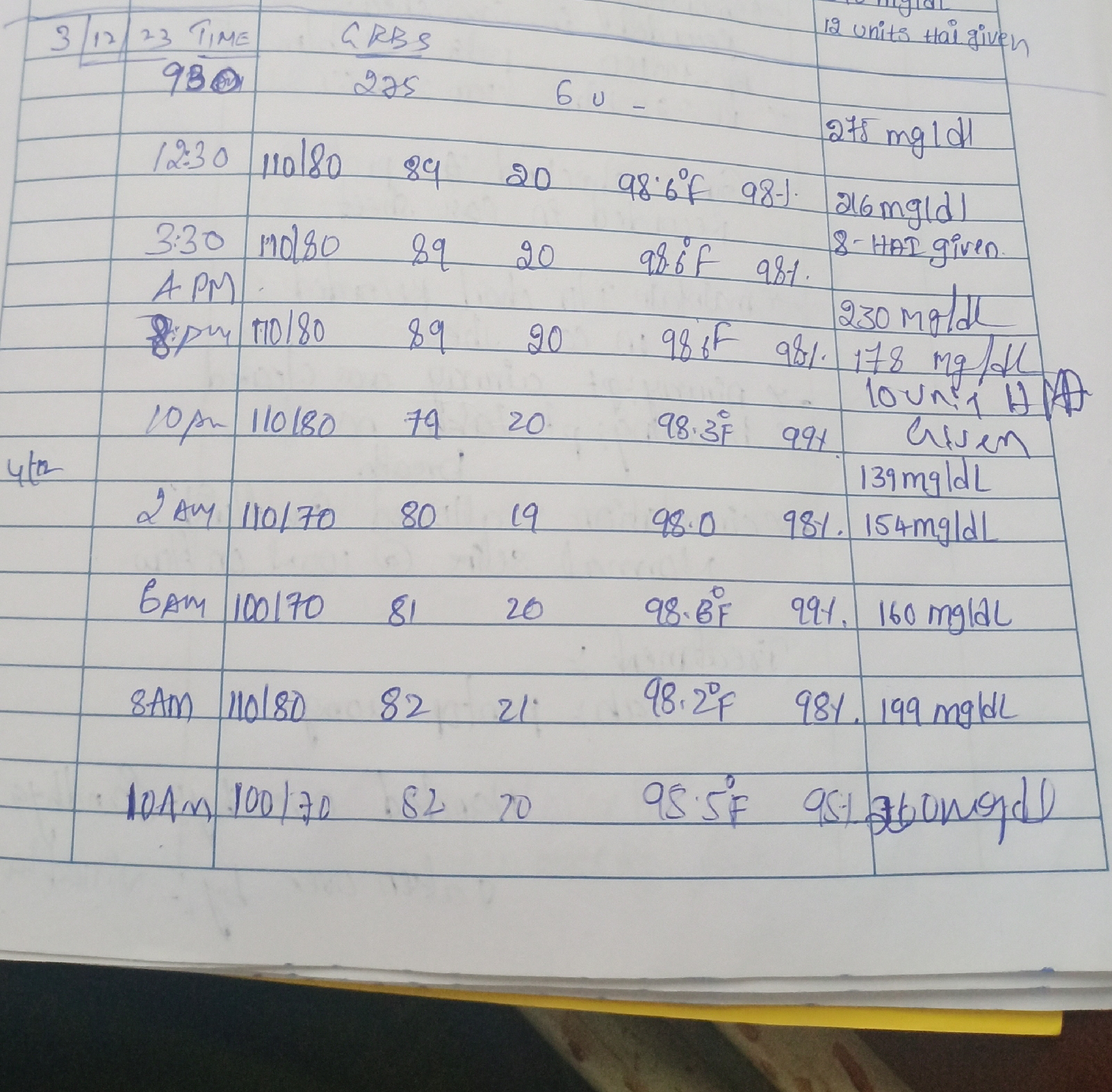
GRBS:- 505mg/dl
On Respiratory system examination:-
On inspection:- normal shaped chest, trachea appears to be in centre, no scars and sinuses present,abdomino thoracic type of respiration, normal respiratory movements present
On palpation:- all inspectory findings are confirmed on palpation.
On percussion:- right. left
Infraclavicular resonant resonant
Mammary resonant . resonant
Axillary. resonant resonant
Infraaxillary. resonant resonant
Suprascapular. resonant. resonant
Infrascapular. resonant. resonant
Upper, mid, lower. resonant. resonant
Interscapular
On auscultation:- normal vesicular breath sounds heard
On CVS examination:-normal JVP, S1,S2 present,no murmurs
2D
Per abdomen:- soft and diffuse tenderness, central umbilicus.
CNS :
Right Handed person.
HIGHER MENTAL FUNCTIONS:
Conscious, oriented to time place and person.
speech : normal
Behavior : normal
Memory : Intact.
Intelligence : Normal
Lobar Functions : No hallucinations or delusions.
MOTOR EXAMINATION:
Right Left
UL. LL. UL LL
BULK Normal Normal Normal Normal
TONE Normal Normal Normal Normal
POWER 4/5. 4/5. 4/5 4/5
SUPERFICIAL REFLEXES:
R. . L
CORNEAL present. present
CONJUNCTIVAL present present
ABDOMINAL present
DEEP TENDON REFLEXES:
R L
BICEPS 2+ 2+
TRICEPS 2+ 2+
SUPINATOR. 2+ 2+
KNEE. 2+. 2+
ANKLE 2+. 2+
SPINOTHALAMIC SENSATION:
Crude touch
pain
temperature
DORSAL COLUMN SENSATION:
Fine touch
Vibration
Proprioception
CORTICAL SENSATION:
Two point discrimination
Tactile localisation.
steregnosis
Graphasthesia.
PROVISIONAL DIAGNOSIS:- Newly diagnosed TYPE II DIABETES MELLITUS with ?UTI with ?cystitis
Investigations:-
Hemogram
Hb:-11.8
TLC:-16400
Platelet:-3.44
APTT:- 34sec
PT:- 17
INR:- 1.2
Blood grouping and Rh typing:- O positive
Serology (HbsAg,HIV,HCV):-Negative
Urine for ketone bodies:- negative
Troponin-I :- 18.3
RFT on 3/12/23:-
Blood urea:- 94
Serum creatinine:-2.2
Serum electrolytes
Na+ 135
K+ 4.8
Cl- 99
Repeat RFT on 4/12/23
Blood urea:- 79
Serum creatinine:- 1.6
Serum electrolytes
Na+ 137
K+ 4.5
Cl- 99
LFT:-
Direct bilirubin :- 1.05
Total bilirubin:- 0.18
SGOT:- 10
SGPT:- 19
Alkaline phosphate:- 336
Total proteins:- 7.9
Albumin: 3.3
A/g ratio:- 0.75
Lipid profile
Total cholesterol:- 205mg/dl
Triglycerides:- 549mg/dl
HDL:- 39mg/dl
Ldl:- 111mg/dl
Cue
Sugars:- ++++
Albumin:- ++
Pus cells:- 3-6 cells
Epithelial cells:- 2-3
Ketone bodies:- positive
HbA1C:- 7.5
FBS after 1 day of admission:- 411mg/dl
Rbs on admission:- 442mg/dl
ABG on admission
Ph:- 7.251
Pco2:- 22.3
PO2:-51.8
O2 sat :- 87.2 %
Repeat ABG
Ph:- 7.341
Pco2:- 23.2
PO2:-106
HCO3 :- 9.4
O2 sat :- 96.7 %
Ortho refferal was done i/v/o back pain and h/o RTA 15 days back
DIAGNOSIS:- URINARY TRACT INFECTION with newly diagnosed type II DM
TREATMENT:-
IV fluids NS @ 100ml/hr
Inj.ceftriaxone 2gm IV BD
Tab.Nitrofurantoin 100mg BD
Inj.Human actrapid insulin s/c TID according to GRBS
Inj.Pcm 1gm IV sos (if temp >101F
Tab.pan 40 mg IV OD
Tab.Etoricoxib 90mg OD
Tab ultracet BD
Voveron gel for local application
Inj.Tramadol 1amp+500 ml NS IV slow over 5 hours
HAI insulin 8IU s/c before breakfast
8IU s/c before lunch
8IU s/c before dinner
- Get link
- X
- Other Apps